Warning this post contains biased content!
If you’re considering using Black Salve as a ‘natural’ alternative skin cancer….think again! Back up on the Black Salve!
As more and more people access Dr Google as their primary health care provider, the potential for misdiagnosis and mistreatment with potentially disastrous consequences looms large, – especially where the controversial Black Salve is concerned.
Skin cancers come in many shapes, sizes and colours and are not always able to be seen with the naked eye. They are sometimes very tricky to diagnose even for a skilled professional, which is why a thorough medical history, skin examination using specialised equipment, biopsy and the skill set of a specialised health professional all contribute to definitively diagnose skin cancer…… even then, some slip through to the gatekeeper.
Don’t believe everything you read on the net!
Living in Queensland, the skin cancer capital of Australia, I see many clients who have successfully sought medical intervention for the removal of their skin cancers with great cosmetic and clinical outcomes but increasingly – and thanks to Dr Google, growing numbers of clients present who have already self diagnosed and initiated treatment of their ‘skin cancers’ with what they have been encouraged to consider to be a more natural treatment option – Black Salve.
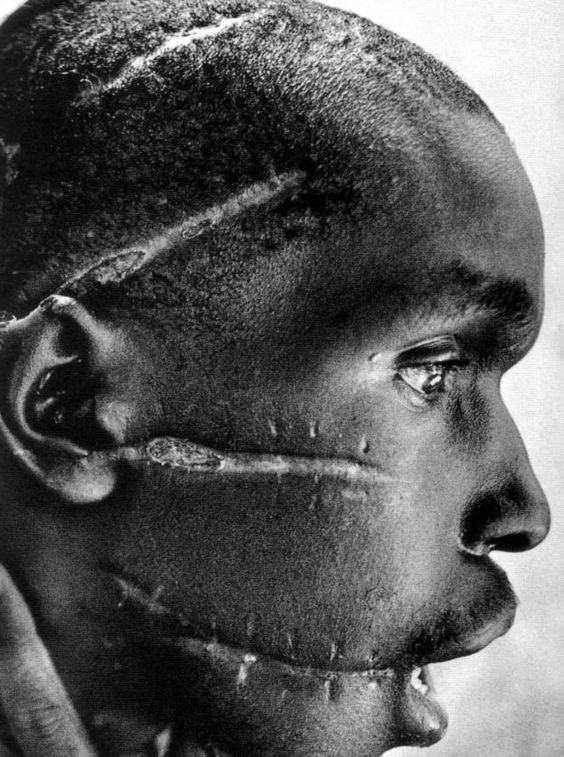
Sadly, I have seen first hand the disastrous cosmetic results of this potentially dangerous practice, which often includes hypo-pigmentation, tissue destruction (and deep, permanent scarring needing surgical revision.
(A quick search on the internet will reveal horrific examples of people with large areas of noses missing after using Black Salve!! – go on I dare you to look.)
Slack jawed I read testimonials on many of Facebook’s Black Salve’s discussion group pages from people offering up well meaning advice on how to treat these strange spots which have recently appeared – ‘what have you got to lose’, or ‘just use it’ are some of the comments which may turn out to be the most terminal advice ever given.
A case study describing Black Salve causality published in 2014 was of a woman diagnosed with melanoma who declined to undergo surgical removal – instead preferring to purchase black salve over the internet – and returning 5 years later with the tragic outcome of metastatic melanoma cancer throughout her body.
What is it and how black salve works…?
Black Salve, Red salve Cansema, blood root, Herbveil8, Can-X, CentreForce ,Curaderm, Hoxsey’s dark red paste, Mexican black salve, and PureCents are all common names and derivatives of Sanguinaria Canadensis (an ammonium salt and alkaloid) derived from the botanical bloodroot, described on the internet as a safe and effective way of treating anything from moles, warts, skin tags to skin cancers.
When mixed with zinc chloride into a paste, and used topically, it creates what is called an eschar. This paste has been described as possessing properties that preferentially targets and kills cancer-affected cells, leaving behind healthy tissues. Most sadly this claim is unfounded in evidence. Its mechanism of action is still unclear but it is thought the bloodroot causes widespread cell death by apoptosis whilst the zinc chloride corrodes the tissue when applied topically. Black salve is like a nuclear missile, indiscriminately, destroying it’s target and everything in it’s path.
An eschar (/ˈɛskɑːr/; Greek: eschara) is a slough or piece of dead tissue that is cast off from the surface of the skin, particularly after a burn injury, but also seen in gangrene, ulcer, fungal infections, necrotizing spider bite wounds, spotted fevers and exposure to cutaneous anthrax.
mmmmm….Not so natural….
When people considering black salve as a natural treatment alternative for skin cancer they may be disappointed to learn Black Salve contains the chemical zinc chloride. Zinc chloride, a known skin irritant, is used in the industrial manufacturing of textiles and metal work and is added to help penetrate the epidermis. It’s a chemical synthesised from zinc and hydrochloric acid and does not generally occur naturally.
Know the Side effects and risks of Black salve
- Obscures tumour identification
- Unconfirmed clearance of cancer cells
- Increase of cancer recurrence or spread
- Destruction and invasion of healthy tissue – imprecise anatamical application of paste resulting in larger than necessary wound and deformity
- Poor cosmetic outcome
- Slower healing
- Greater risk of complications due to infection
- Open wound
- Hypopigmentation
- Deficits- hollows in the skin due to dermal and subcutaneous tissue destruction
Tip: the longer a wound takes to heal the increased risk of scarring
What the authorities say….
Although our Therapeutic Goods Australia (TGA) regulatory body have not banned the use of Black Salve in Australia, they have strongly advised against the use of black salve or any of its derivatives.
We know early detection and accurate diagnosis goes a long way in reducing preventable deaths from skin cancer. The use of black salve may increase the risk of diagnostic delay by obscuring cancers and delaying appropriate treatment
As a skin health professional I always try to advocate for my readers and provide content enabling you to make informed decisions based on evidence-based research. Based on this philosophy, I unequivocally recommend against the use of Black Salve….the risks and side effects are not in favour of Black Salve when treating skin cancer!
Have you had any experience with Black Salve?