It’s all fun and games until you end up over the handle bars of your bike….scenes of tears, scars or worse, Brad Pitt-less – that is if you’re Angelina! Unless you live in a bubble or are Teflon coated, chances are you won’t have a skin which is ‘Scar Free’. Whether from surgery, pool dives gone wrong, cuts, stretchmarks or even acne; scars are an inevitable tracing of a life well lived. Wherever the skin has been broken and needs to repair itself, there will be a story to be told with a scar.
Defintion:Scar – a mark left on the skin or within body tissue where a wound, burn, or sore has not healed completely and fibrous connective tissue has developed.
Any injury to our skin can result in a temporary or sometimes unwelcome permanent scar. If it’s not a conversation opener at a dinner party, we spend a lot of time disguising, covering or wanting to get rid of them.
Unlike the gorgeous Kate Middleton, your scar isn’t hidden beneath your hairline, there are a number of scar minimisation treatment options available to help reduce the appearance of those unwanted scars.
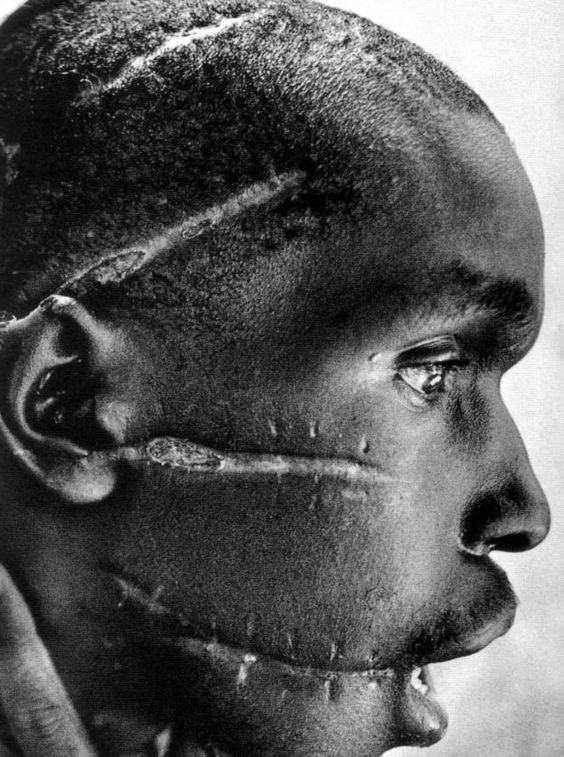
Skin heals unpredictably and so it can tough to predict the nature and extent of scarring after an injury or operation. Multiple factors including skin type, age, health status and the depth and nature of the injury to the skin all contribute to how a scar heals and what residual signs or scars may be left. Different skin types also have an impact on how the skin heals For example, Asian or darker skin types have an increased risk of developing keloid, hypertrophic scarring or post inflammatory hyper pigmentation.
First up….Types of scars
Mature scars are scars which have completed the healing process. These types are definitely more challenging to treat.
Flat scars are scraped knees, abrasions or common superficial injuries.
Atrophic scars are indented or depressed scars where and include the destruction of the supporting structure of the dermis- seen in post acne scarring.
Keloid or Hypertrophic scars occur from superficial to deep injury of the skin and more commonly affect darker skin types or those with an Asian descent. They may undergo surgical revision with no guarantee of resolution. Keloid scars usually occur from the chest up, where scar tissue grows outside the borders or boundaries of the original scar or injury – seen in tribal markings or facial piercings.
Hyper-pigmentation This is where there is a darkening of the skin caused by an increase in melanin production in the post inflammatory phase of a wound repair. Sun exposure during the healing process can exacerbate this.
Hypo-pigmentation is a loss of melanin to the site of injury and may be permanent or temporary depending on the depth of injury.
Early tip; Before that scar horse bolts…… Good wound care and scar prevention is always better than seeking scar minimisation treatment options.
A quick tour on how the skin heals…
There are three phases in wound healing and they all overlap each other ultimately resulting in the healing of a wound-
Inflammatory phase– the bodies first response, is to stop the bleeding and send in it’s army of protective cells to ward off infection as well as cells that will direct the healing process .
Proliferation phase– is the crucial rebuilding stage where epithelial cells (skin cells) resurface the wound — seen in a scab.
Maturation phase– this is the final stage and the replacement of collagen from type III to type 1.During this phase erythema or redness decreases. This phase may take up to 2 years to complete.
Myth busting….A common misconception is that wounds should be air dried and a scab allowed to form. Recent studies now confirm that keeping wounds moist and covered with dressings not only reduces pain and the risk of infection but also results in faster healing times when compared to dry wound healing.
Tip; A quicker a wound heals the less of a scar it will form.
You’ve got that Scar now what?
Treatments explained….
- Sunscreen – Sun protection is vital for minimising the appearance of scars preventing hyper or hypo pigmentation – Use a broad-spectrum sunscreen to protect against UVA and UVB rays.
Tip; the zinc in broad-spectrum sunscreens has great healing properties in addition to sun protection.
- Massage the wound gently – this helps in breaking down and lessons the risk of thick scarring from forming. Massaging should only be performed during the maturation phase of healing.
- Retinols – when applied topically these Vitamin A derivatives help to control hyperpigmentation whilst facilitating cell renewal.
- Silicon gel sheeting – Putting a sheet of silicon gel on a scar every day may help it fade or keep it from getting worse. The sheeting is available at pharmacies or from dermatologists and should be used for at least 3 months.
- Concealer – A quick fix! Pick a shade that is waterproof and most effective with the colour of your scar and skin tone. For a pink scar use concealer with green undertones, for a brown scar, try a concealer with a yellow undertones.
- Bleaching creams – May be effective for dark hyper pigmented scars.
- Dermal fillers – Injecting substances such as collagen or fat can immediately raise sunken atrophic scars. However, this treatment isn’t permanent and may need to be repeated regularly to maintain benefit.
- Steroid injections – These may help flatten raised scars, but a long-term course may be needed note-Long term use of steroids in the skin may also cause a thinning of the skin.
- Dermabrasion – This procedure abrades the surface of the skin,helping to reduce the look of raised scars.
- Microdermabrasion – a less invasive process, helping superficial scarring.
- Laser resurfacing – The skin surface is removed with lasers, or lasers are used to work on the collagen in the dermis without removing the upper layer of skin.
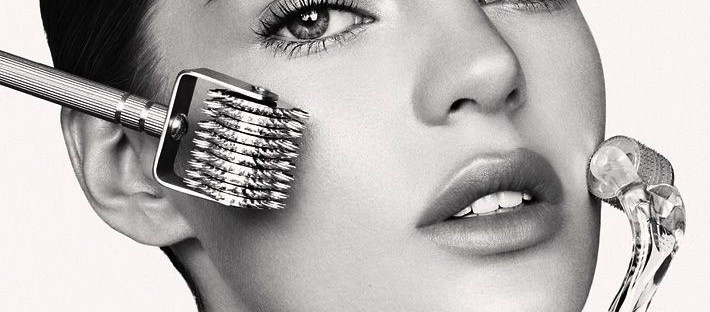
- Micro-needling – Small needles are delivered into the dermal layers of the skin, to break down scar tissue and stimulate the formation of new collagen.
- Subcision – The sharp edge of a hypodermic needle is used to break down fibrous connective strands underneath the scar to improve appearance .
- Surgery – You can’t remove a scar entirely with surgery, but you can alter its size, depth, or colour. Surgery isn’t suggested for hypertrophic or keloid scars because it can make them worse.Consult with an experienced Plastic Surgeon or Cosmetic Surgeon prior to considering this option.
The good news is scars do resolve themselves significantly over time but some may never completely disappear.It’s good to know however, that for those people who can do without the permanent reminder of a life well lived, there are many scar minimisation treatment options available.
Have you had any success with removing scars?
Susan x