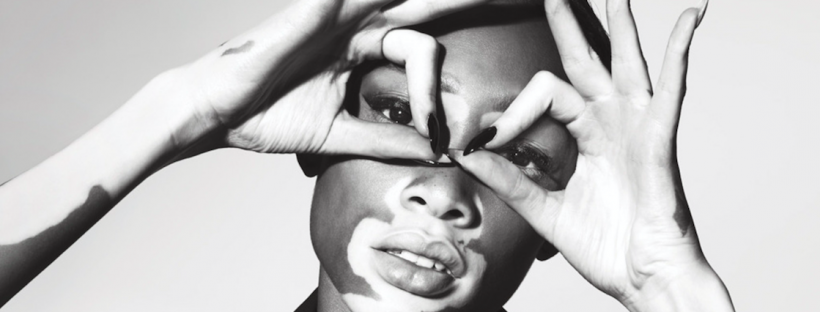
Recently strutting the catwalk at this years New York fashion week was newest model sensation Winnie Harlow: aka Chantell Young- Brown.The 20-year-old Canadian model first making headlines when she competed in America’s nxt top model.
Recently strutting the catwalk at this years New York fashion week was newest model sensation Winnie Harlow: aka Chantell Young- Brown.The 20-year-old Canadian model first making headlines when she competed in America’s nxt top model.
Headline making because not only is she strikingly beautiful but she also suffers from an acquired skin disorder called Vitiligo.
The most common onset age of Vitligo ranges from 10-30 years of age. Whilst Winnie was first diagnosed when she was just 4 years old, she recalls growing up in Toronto, being bullied – not so now – with fans all over the world using makeup to mimic her look!
Far from the bullying childhood taunts of ‘cow and zebra’, Winnie is now celebrating her diversity, thanks to a lucrative contract with fashion label Desigual , and has gone on to become the spokeswoman for Vitiligo sufferers with fans now applying makeup to mimic her look.
Whilst Michael Jackson –a Vitlitgo sufferer himself -sang ‘It doesn’t matter if you’re black or white’ ….for some sufferers it does matter!
Whilst Winnie is comfortable in her own skin, not all sufferers share this confidence, with a high incidence of depression being diagnosed amongst sufferers.
So what is it?
leuko = white / derma = skin
Vitiligo presents with milky white areas of depigmentation increasing in size and migrating to other areas of the body. This depigmentation occurs when the melanocytes, which produce skin colour, cease functioning normally. Originating on the face, hands and bony prominences such as knees and elbows, these depigmented patches affect up to 2% of the population worldwide and seems to be more prevalent in darker skin types.
It’s origin is not fully understood but a lot of studies support a diagnosis of an autoimmune disorder.
In addition to the autoimmune component of Vitiligo it may also be triggered by sunburn, stress, genetics, viral infections or physical trauma to the skin.
There are 2 types of treatment options available for Vitiligo – surgical and non-surgical. As with most diseases early intervention is often the most successful when it comes to Vitiligo.
Non- surgical
Phototherapy
- the skin is exposed to UVB light 2-3 times a week ( not consecutive days )
- may be used safely in children.
- a 2009 study showed taking oral Vit E may increase the effectiveness of UVB phototherapy
- is widely used and can result in satisfactory repigmentation in up to 70% of patients when an early diagnosis is made.
adverse side effects – temporary itching and dry skin
Photochemotherapy
- involves the use of psoralens in combination with exposure to UVA light
- psoralens increase the skin’s sensitivity to UV light and.the absorption of UV rays —
- psoralens may be taken orally or applied topically followed by exposure to UV light
- 2-3 treatments per week and anywhere from 50 – 300 treatments are needed for repigmentation
adverse side effects – an increased risk of skin cancer; nausea sometimes associated with taking oral psoralens; sunburn type reactions; freckling
Immune mediators
- topical creams containing calcineurin inhibitors; 0.1% tacrolimus and 1% pimecolimus applied twice daily
- their mechanism of action is to prevent the body’s T cells attacking and destroying it’s own melanocytes (pigment containing cells)
- prevents the inflammatory responses.
- alternatives to topical steroids due to efficacy and lack of side effects.
Steroid therapy
- topical steroidal creams applied twice daily for up to 1 year
adverse side effects – skin atrophy or thinning of the skin; the addition of Vit A with steroidal cream may help to reduce skin atrophy .
Depigmentation therapy
- should be carefully considered as depigmentation is a permanent treatment option.
- results may take from 3 months to a year
- twice daily application, topical cream containing, monobenzone. –
- depigmentation is gradual and achieved through the destruction of the melanocytes.
- bleaches the unaffected skin blending the patches
Adverse reactions – increased risk of skin cancer; sun safety must be adhered to at all times to avoid sunburn; redness, swelling, itching and dry skin
Laser Therapy
- quicker response time
- used in conjunction with Vit D
Skin Camouflage
- mild cases makeup may be used to disguise the depigmented patches
- avoidance of tanning which may darken the surrounding skin.
Micropigmentation
- similar technique to tattooing
- colour matching is poor
- colour fading over time
Surgical treatment options
- grafting and transplanting skin from non affected areas
- up to 85% of sufferers have seen repigmentation
- longevity is unknown.
Alternative options – Chinese Medicine
- treatments include the use of psoralens in conjunction with UVA therapies
- herbal preparations targeting autoimmune disorders
For support and worth checking out if you want more information …
https://www.facebook.com/The-Vitiligo-Girl-TJ-151344275055276/timeline/
https://www.vitiligosupport.org
The treatment options I’ve listed are treatments cited from a review article ,Yanfei Zhang et al ‘Vitiligo nonsurgical treatment:a review of latest treatment researches’ Dermatologic Therapy, Vol. 27, 2014, 298–303 accessed 10th October 2015
{http://eds.a.ebscohost.com/eds/pdfviewer/pdfviewer?vid=6&sid=9bbb3e53-ddaf-4961-bdc8-0a090f2fcc95%40sessionmgr4002&hid=4213}
ASkinSolutions x
If you have a skin health question you need answered drop me a line!